How to Identify Early Signs of a Slipped Disc
A slipped disc, also known as a herniated disc or prolapsed intervertebral disc, is one of the most common spinal issues among working-age adults, particularly those aged 30 to 60. In India, sedentary lifestyles, desk-bound jobs, and a lack of ergonomic awareness have contributed to the rising prevalence of spine-related disorders.
Understanding the early signs of a slipped disc can help prevent chronic pain, nerve damage, or the need for surgical intervention. This guide outlines how to recognize symptoms early, explains why they occur, and clarifies what steps to take next.
What Is a Slipped Disc?
Your spine is made up of vertebrae, each separated by soft, jelly-like cushions called intervertebral discs. These discs absorb shock and allow flexibility.
A slipped disc occurs when:
The outer layer (annulus fibrosus) of the disc weakens or tears, and
The inner gel-like core (nucleus pulposus) bulges or leaks out.
This displaced disc material can compress spinal nerves, leading to pain, numbness, and other neurological symptoms.
Common Locations:
Lumbar Spine (Lower Back) – most commonly affected.
Cervical Spine (Neck) – also frequently involved.
Thoracic Spine (Upper Back) – rare but possible.
Why Early Detection Matters
Identifying a slipped disc in its early stages increases the chances of successful non-surgical treatment. If left unaddressed, a herniated disc can:
Cause persistent nerve pain.
Lead to muscle weakness or functional impairment.
Progress into spinal stenosis or chronic disability.
Early Signs and Symptoms of a Slipped Disc
The symptoms of a slipped disc depend on its location and the nerves involved. Here are the most common early indicators:
1. Localized Back or Neck Pain
Dull or sharp pain in the back or neck.
Pain may worsen with movement, sitting, or lifting.
Often the first symptom, especially in the lumbar spine.
2. Radiating Pain (Nerve Root Pain)
Also known as radiculopathy.
Pain may travel from the lower back to legs (sciatica) or from the neck to shoulders/arms.
Often described as burning, shooting, or electric.
3. Numbness or Tingling
Common in hands, arms, buttocks, or legs.
Indicates nerve compression.
Often starts mildly and may be ignored early on.
4. Muscle Weakness
Weak grip, foot drop, or difficulty lifting objects.
Muscle fatigue during simple tasks (e.g., climbing stairs).
May indicate the nerve signal to the muscle is compromised.
5. Worsening Pain After Prolonged Sitting or Standing
Disc pressure increases when sitting.
Standing or walking may also trigger pain, depending on disc location.
6. Reduced Range of Motion
Difficulty bending forward, backward, or rotating the neck.
Stiffness in the spine that limits daily activities.
What Causes a Slipped Disc?
Understanding the root causes can help you modify lifestyle risk factors. Here are the main contributors:
1. Age-Related Degeneration
Disc material loses hydration and elasticity with age.
Most common in people over 30.
2. Poor Posture and Sedentary Lifestyle
Long hours at desks without back support.
Forward head posture while using phones or laptops.
3. Improper Lifting Techniques
Lifting heavy weights without bending the knees.
Sudden twisting movements.
4. Repetitive Strain
Jobs requiring frequent bending, pushing, or pulling.
Sports with excessive spinal loading (e.g., weightlifting).
5. Obesity
- Excess body weight increases pressure on spinal discs.
6. Smoking
- Impairs disc nutrition and accelerates degeneration.
Risk Factors Specific to Indian Adults
In the Indian context, certain cultural and occupational factors elevate the risk:
Prolonged cross-legged sitting on the floor.
Two-wheeler driving on uneven roads.
Manual labor without ergonomic practices.
Limited access to preventive spine care in semi-urban and rural areas.
How a Slipped Disc Is Diagnosed
1. Clinical Examination
Orthopedic or spine specialists assess mobility, posture, reflexes, and muscle strength.
Neurological tests may identify areas of numbness or weakness.
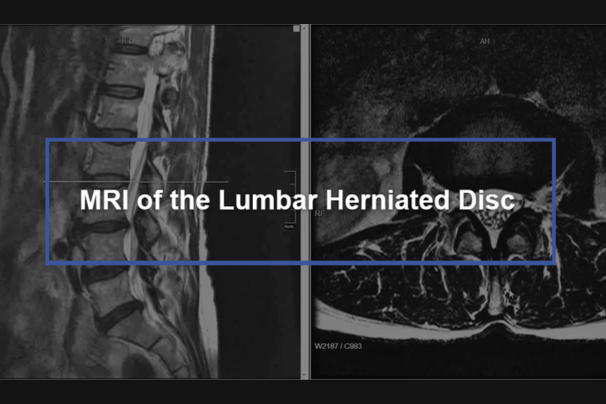
2. MRI Scan (Magnetic Resonance Imaging)
Gold standard for diagnosing disc herniation.
Shows disc position, nerve compression, and spinal canal involvement.
3. CT Scan
- Useful in evaluating bony structures if MRI is contraindicated.
4. Electromyography (EMG)
Assesses electrical activity in muscles.
Helps confirm if symptoms are nerve-related.
When to See a Doctor Immediately
Not all back pain is serious, but the following red flags require urgent evaluation:
Severe or unrelenting pain not relieved by rest.
Pain radiating below the knee or into the arm.
Sudden numbness or weakness in limbs.
Loss of bladder or bowel control (possible cauda equina syndrome).
History of cancer, trauma, or steroid use with new back pain.
Preventive Steps for Spine Health
Even if symptoms are mild, early care can prevent complications. Focus on:
1. Ergonomic Corrections
Use chairs with lumbar support.
Keep computer screens at eye level.
Maintain neutral spine alignment while sitting or standing.
2. Regular Movement
Avoid sitting for more than 30–45 minutes at a stretch.
Incorporate standing desks or walk breaks.
3. Strengthening Exercises
Core muscle strengthening supports the spine.
Practice under supervision of a trained physiotherapist.
4. Weight Management
- Maintain healthy BMI to reduce spinal stress.
5. Spinal Screenings
- Periodic evaluation by a spine specialist helps detect early degeneration.
Non-Surgical Treatment Options
Many patients recover from a slipped disc without surgery if caught early. Common approaches include:
1. Physical Therapy
- Tailored exercises to relieve pressure and improve function.
2. Medication
NSAIDs (Non-steroidal anti-inflammatory drugs) for pain and inflammation.
Muscle relaxants as needed.
3. Epidural Steroid Injections
- Used in selected cases for pain relief when conservative care fails.
4. Posture and Lifestyle Modifications
- Part of long-term prevention and healing.
Note: Surgery is recommended only if there is severe nerve compression, motor weakness, or failure of conservative therapy over several weeks.
Conclusion: Stay Informed, Act Early
Recognizing the early signs of a slipped disc is crucial for timely treatment and long-term spine health. In most cases, early intervention using conservative methods can reverse symptoms, prevent nerve damage, and avoid surgery.
At WeAreSpine, medical professionals stress the importance of awareness, early diagnosis, and evidence-based care. If you suspect any of the symptoms listed above, consult a spine specialist promptly and begin your recovery journey with informed steps.
FAQs
Q. Is a slipped disc permanent?
No, many cases resolve with proper treatment. Early-stage herniations often heal with rest and therapy.
Q. Can you exercise with a slipped disc?
Yes, but under the guidance of a specialist. Specific exercises help reduce pain and improve mobility.
Q. Will I need surgery?
Most patients don’t need surgery. However, if symptoms persist or worsen despite conservative care, surgery may be necessary.
Q. Can slipped discs recur?
Yes. But adopting healthy habits, posture correction, and core strengthening can reduce recurrence risk.