Neck pain has silently become one of the most common health complaints of the modern era. With the surge in desk jobs, smartphone usage, and screen-based lifestyles, more people are reporting stiffness, aches, and recurring discomfort in the neck. What often begins as a minor inconvenience is sometimes a sign of a more serious spinal condition known as cervical spondylosis.
Cervical spondylosis refers to the wear and tear of the bones, discs, and joints of the neck (cervical spine). While it is primarily age-related, lifestyle factors have accelerated its onset. According to the Mayo Clinic, more than 85% of people over 60 years show signs of cervical spondylosis on imaging. But in India, studies have revealed that young professionals in their late 20s and 30s are increasingly being diagnosed due to prolonged screen exposure, poor posture, and lack of spinal care.
Why is this concerning? Because ignoring the early signs allows the condition to progress silently. Over time, it may lead to nerve compression, spinal cord involvement, and significant disability. Recognizing the early red flags and acting upon them is key to prevention and management.
This blog will explore the science, symptoms, diagnosis, and treatments of cervical spondylosis, with practical lifestyle and ergonomic advice, and highlight why Indians in particular must take this condition seriously.
Understanding Cervical Pain
Cervical spondylosis, also called cervical osteoarthritis or neck arthritis, is a degenerative condition of the cervical spine.
The cervical spine consists of:
- Seven vertebrae (C1–C7): The bones forming the neck portion of the spine.
- Intervertebral discs: Soft cushions between vertebrae acting as shock absorbers.
- Facet joints and ligaments: Supporting structures that allow movement and stability.
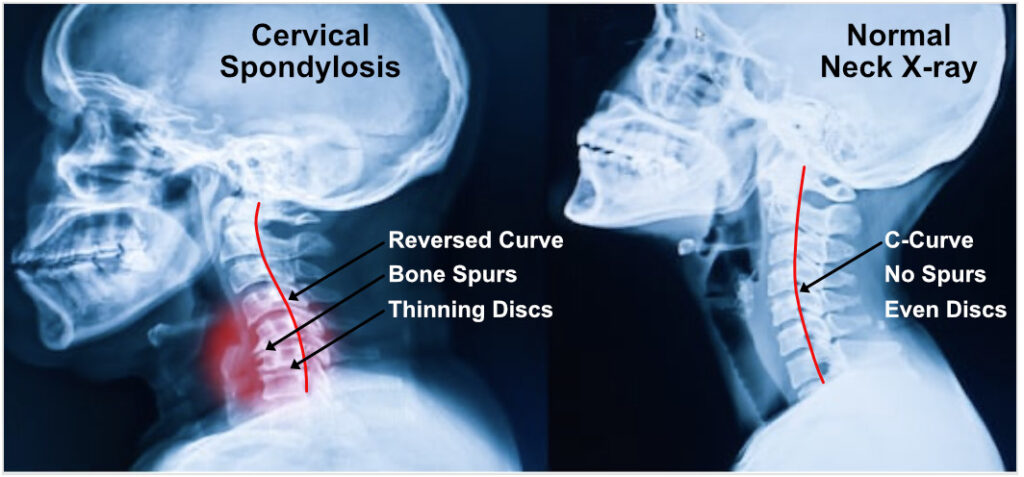
Over time, these structures undergo degeneration due to aging, repetitive strain, or injury. Key changes include:
- Disc dehydration and shrinkage, reducing cushioning.
- Bone spurs (osteophytes) developing as a compensatory response.
- Ligament stiffening, which reduces flexibility.
- Joint cartilage wear, leading to stiffness and inflammation.
While mild degeneration is considered a part of aging, when it progresses to symptoms such as pain, nerve compression, or restricted mobility, it is clinically diagnosed as cervical spondylosis.
Why Early Recognition is Crucial
Cervical spondylosis often develops slowly. At first, symptoms may appear mild or intermittent, such as neck stiffness after a long day at work. Many people dismiss these as “normal” aches. However, untreated spondylosis may worsen, leading to complications such as:
- Cervical radiculopathy: Pinched nerve causing pain, tingling, or weakness in arms/hands.
- Cervical myelopathy: Compression of the spinal cord leading to balance problems, coordination issues, or even bladder/bowel dysfunction.
- Chronic disability: Severe stiffness and mobility restriction.
Early identification and management — often with non-surgical treatments like physiotherapy and ergonomics — can stop progression and restore quality of life.
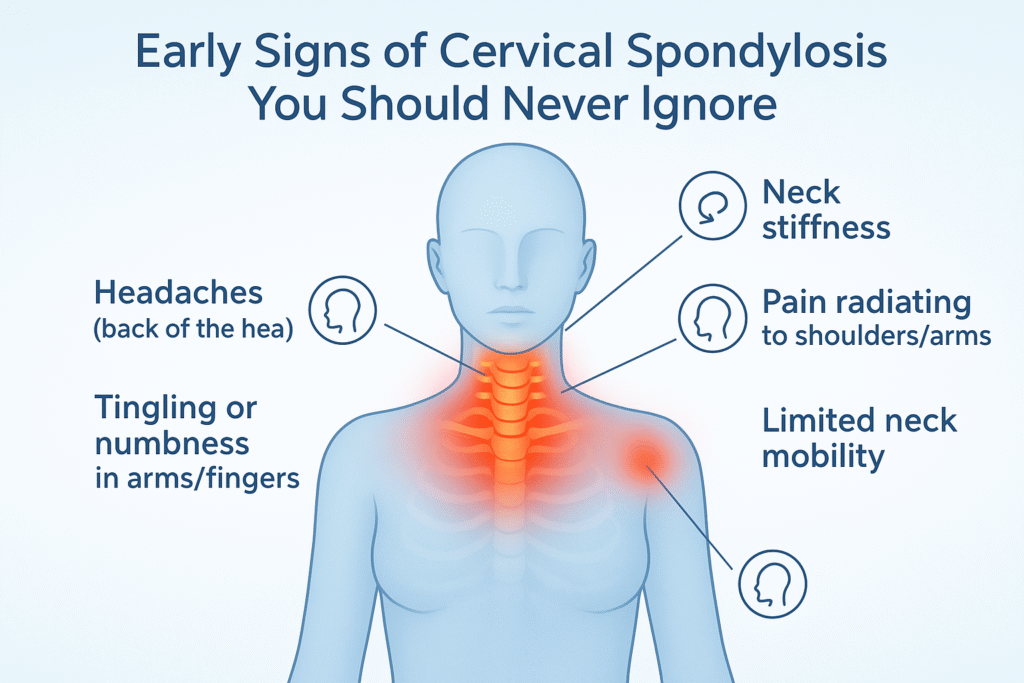
Early Signs of Cervical Spondylosis You Should Never Ignore
Here are the most common warning signals backed by medical literature (NIH, Mayo Clinic, PubMed):
1. Persistent Neck Stiffness
- A hallmark symptom.
- Patients describe it as difficulty moving the head freely.
- Worse in mornings or after long sitting sessions.
2. Frequent Headaches (Cervicogenic Headaches)
- Originating from neck strain.
- Pain radiates from base of skull to forehead.
- Often misdiagnosed as migraines or tension headaches.
3. Shoulder and Arm Pain
- Pain radiating from the neck to shoulder/arm.
- Suggests nerve root irritation.
- Sometimes sharp, sometimes dull ache.
4. Tingling or Numbness in Hands and Fingers
- Indicates nerve compression.
- May affect grip strength and fine motor skills.
5. Grinding or Popping Sounds (Crepitus)
- Audible clicks or grinding with neck motion.
- Sign of cartilage wear and bone spur friction.
6. Reduced Neck Mobility
- Difficulty turning head sideways.
- Restricted motion during driving or looking up/down.
7. Muscle Weakness
- Weak grip, dropping objects.
- Caused by long-standing nerve impingement.
8. Dizziness and Balance Issues
- Less common but significant.
- Related to cervical myelopathy or vascular compromise.
9. Fatigue and Sleep Disturbances
- Chronic pain disrupts sleep cycles.
- Leads to daytime tiredness and reduced productivity.
Risk Factors
According to Harvard Health, WHO, and NIH, key risk factors include:
- Age: Most common over 40–50 years.
- Occupation: IT professionals, drivers, teachers, students with long screen hours.
- Posture: Slouching, forward head posture, prolonged laptop/mobile use.
- Smoking: Accelerates disc degeneration.
- Genetics: Family history of osteoarthritis.
- Injuries: Previous trauma to the neck.
- Lack of exercise: Weak supporting muscles worsen degeneration.
If symptoms persist, medical evaluation is essential. Standard diagnostic tools include:
- Physical examination: Testing reflexes, muscle strength, range of motion.
- X-rays: Reveal bone spurs, disc height loss.
- MRI: Shows disc bulges, nerve or spinal cord compression.
- CT scans: For detailed bone structure.
- Electromyography (EMG): Measures nerve electrical activity.
Treatment Options
Non-Surgical Approaches (First Line)
- Physiotherapy: Stretching, strengthening, posture retraining.
- Medications: NSAIDs, muscle relaxants.
- Heat/Ice therapy: Relieves stiffness.
- Cervical collars (short-term): For acute pain flare-ups.
- Lifestyle modifications: Ergonomic seating, screen breaks.
Surgical Approaches (For Severe Cases)
- Discectomy: Removal of herniated disc.
- Laminectomy: Decompression by removing bone.
- Spinal fusion: Stabilization of vertebrae.
Surgery is rare and reserved for severe neurological impairment.
Lifestyle and Self-Care for Prevention
Ergonomic Practices
- Keep screens at eye level.
- Use chairs with proper lumbar and neck support.
Take 5-minute breaks every 30–40 minutes.
Exercises (Medically Recommended)
- Neck stretches: Side bends, rotations.
- Chin tucks: To correct forward posture.
- Shoulder blade squeezes: Strengthen upper back.
Nutrition
- Calcium and Vitamin D for bone strength.
- Omega-3 fatty acids (flaxseeds, walnuts) for anti-inflammatory effect.
- Magnesium and protein for muscle and disc health.
Sleep Hygiene
- Use orthopedic pillows.
- Avoid sleeping on stomach.
- Keep neck aligned with spine.
Cervical Spondylosis in India: An Emerging Epidemic
A study conducted at AIIMS, New Delhi found a significant increase in cervical spondylosis cases among IT professionals under 40 years. Prolonged sitting, poor ergonomics, and mobile phone use were key contributors.
Additionally:
- Rural women carrying heavy loads on their heads experience accelerated cervical degeneration.
- Drivers and manual laborers face repetitive neck strain.
This dual urban-rural burden highlights the urgent need for awareness, preventive physiotherapy, and workplace ergonomics in India.
Myths vs Facts
- Myth 1: Only old people get cervical spondylosis.
Fact: Younger adults are increasingly being diagnosed due to posture and lifestyle. - Myth 2: Neck pain always means cervical spondylosis.
Fact: Many causes exist, including muscle strain, herniated discs. Only imaging confirms diagnosis. - Myth 3: Surgery is the only treatment.
Fact: Over 90% cases improve with conservative management. - Myth 4: Resting completely is best.
Fact: Prolonged inactivity weakens muscles. Controlled movement and physiotherapy help recovery.
When to See a Doctor Immediately
- Severe pain not improving with rest.
- Weakness or numbness in arms/legs.
- Loss of bladder/bowel control.
- Sudden dizziness or balance loss.
These are red flag symptoms of spinal cord involvement and need urgent evaluation.
Role of Physiotherapy
Physiotherapy is considered the cornerstone of management:
- Restores flexibility.
- Strengthens supporting muscles.
- Reduces nerve compression symptoms.
- Educates patients on posture and ergonomics.
How We Are Spine Can Help
At We Are Spine, the focus is on comprehensive, patient-centered spine care. The expert team of spine specialists and physiotherapists use a combination of:
- Accurate diagnostics with advanced imaging.
- Customized physiotherapy programs tailored to each patient.
- Lifestyle and ergonomic guidance for sustainable results.
- Minimally invasive techniques if surgery becomes unavoidable.
This approach ensures not only treatment of existing pain but also long-term prevention and better quality of life.
Conclusion
Cervical spondylosis may start subtly — a stiff neck after a long day, a headache that lingers, or a strange tingling in the fingers. These may seem minor, but they are often the body’s early warning system.
Recognizing the early signs, seeking timely medical advice, and adopting preventive strategies can stop the disease in its tracks. To explore professional care options, you can learn more about cervical spondylosis treatment and how targeted interventions can improve neck health.
In a country like India, where screen time, sedentary jobs, and heavy manual labor coexist, awareness is crucial. With proper posture, regular breaks, exercises, and timely care, cervical spondylosis does not have to control your life.
Your spine health is in your hands — listen to your body, respect the early signals, and take action before it’s too late.
I have just been diagnosed with Cervical Spondylosis. I want to learn everything and get started doing what I need to do. This article really helped me to know that I am at the beginning and maybe not at the end. I am interested in any other information you have.