Spine health in women is a critical yet often overlooked aspect of overall well-being. Back pain is one of the leading causes of disability globally—and among the people affected, women make up a disproportionately large share. While anyone can suffer from spinal problems, women face unique biological and physiological challenges that make them more susceptible. From the stress of pregnancy to the silent progression of osteoporosis and the impact of hormonal changes, the spine often bears the burden of life transitions that are specific to women.
At WeAreSpine, we recognize the gender-specific nuances of spinal health. Our commitment to evidence-based care, minimally invasive treatment options, and rehabilitation protocols tailored for women ensures that we meet the needs of women at every stage of life. In this blog, we take a detailed look at why women are at higher risk for back issues and what steps they can take to protect their spine health.
Why Women Are More Prone to Back Issues
There isn’t a singular cause behind why women face more back issues—rather, it’s the result of a combination of anatomical, hormonal, and lifestyle factors. Here’s a closer look:
Hormones play a key role in bone health, muscle elasticity, and pain sensitivity. For women, hormonal fluctuations across different life stages can directly impact spinal integrity:
- Menstrual cycle: During menstruation, changes in estrogen and progesterone levels can increase muscle tension and pain perception, leading to temporary backaches or increased discomfort from existing spinal issues.
- Perimenopause and menopause: The drop in estrogen levels during this phase affects bone mineral density and the hydration of intervertebral discs. This speeds up disc degeneration and loss of bone mass, which can lead to conditions like degenerative disc disease and osteoporosis.
- Ligament laxity: Estrogen influences ligament flexibility. When hormone levels fluctuate, ligaments supporting the spine may weaken, making the spine more vulnerable to injury.
Fact: According to the International Osteoporosis Foundation, 1 in 3 women over age 50 will experience osteoporotic fractures in their lifetime.
2. Pregnancy and Postpartum Strain
Pregnancy is a uniquely female experience that introduces a wide range of spinal stresses:
- The growing fetus shifts a woman’s center of gravity, increasing lumbar lordosis, which is a leading cause of lower back pain during pregnancy.
- The hormone relaxin, released during pregnancy, softens ligaments and joints to prepare for childbirth—but also reduces spinal stability.
- Postural changes, prolonged standing, lifting toddlers, and improper nursing posture continue to stress the back even after childbirth.
Clinical Insight: Studies suggest that more than 50% of pregnant women experience significant back pain, and in many cases, it can continue postpartum if not managed with proper physiotherapy and spinal care.
Osteoporosis is a silent condition that often goes unnoticed until a fracture occurs. Women are significantly more affected than men, primarily due to the loss of protective estrogen after menopause.
- Bone density loss begins in the mid-30s but accelerates after menopause.
- The vertebrae, being porous and lightweight, are particularly vulnerable to fractures.
- Compression fractures can occur with minor trauma or even routine activities like bending or lifting light objects.
Symptoms of spinal compression fractures may include:
- Sudden or severe back pain
- Loss of height over time
- A hunched forward posture (kyphosis)
At WeAreSpine, our spine specialists offer non-invasive treatments like vertebroplasty, along with bone health monitoring to manage such conditions proactively.
Spine Conditions That Commonly Affect Women
Let’s examine some specific spinal conditions where women are at higher risk:
A. Degenerative Disc Disease
Aging, hormonal imbalances, and physical stressors accelerate disc dehydration and degeneration, especially in women. Symptoms include:
- Chronic lower back or neck pain
- Numbness or tingling in limbs
- Pain aggravated by movement
B. Spinal Osteoarthritis
More prevalent in postmenopausal women, this condition affects the facet joints of the spine, causing:
- Joint stiffness
- Morning back pain
- Decreased range of motion
C. Sacroiliac (SI) Joint Dysfunction
The SI joint connects the spine to the pelvis. It becomes unstable or inflamed during pregnancy or after childbirth due to ligament stretching and postural changes. Women may feel:
- Pain in the lower back, hips, or buttocks
- Discomfort while climbing stairs or standing from a seated position
D. Scoliosis in Women
Adult-onset scoliosis, often due to degenerative changes, is more frequent in women. In addition to visible curvature, it may lead to:
- Nerve compression
- Uneven hips or shoulders
- Mobility limitations
Spine Health Across a Woman’s Life Stages
Spinal health is not static—it changes across a woman’s lifespan. Here’s how to monitor and manage spine health at different ages:
Adolescence and Early Adulthood
- Carrying heavy school bags
- Poor screen-time posture
- Participation in sports without proper warm-up
Prevention tip: Encourage strength training and proper posture education from an early age.
Reproductive Years (20s–40s)
- Hormonal fluctuations affect joints and ligaments.
- Pregnancy and caregiving activities place strain on the back.
- Sedentary desk jobs contribute to poor spinal ergonomics.
Actionable advice: Invest in ergonomic furniture, regular exercise, and pre/postnatal physiotherapy.
Postmenopausal Years (50+)
- High risk of osteoporosis and fractures.
- Muscle mass and flexibility decline.
- Weight gain and inactivity aggravate spine issues.
Management strategies: Regular bone density scans, calcium & vitamin D supplements, and tailored physiotherapy routines.
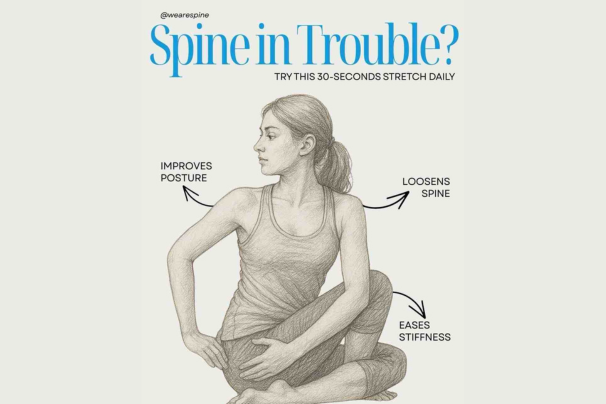
Prevention and Lifestyle Tips for Long-Term Spine Health in Women
Spine health is not just about treatment—it’s about prevention and maintenance. Here are some key tips tailored for women:
1. Stay Physically Active
- Engage in weight-bearing exercises like walking or light jogging.
- Practice yoga or Pilates to strengthen core muscles.
- Avoid prolonged inactivity, which weakens spinal support.
2. Focus on Posture
- Sit upright with lumbar support.
- Adjust screen height to avoid neck strain.
- Carry bags with two straps or use trolleys instead.
3. Maintain Healthy Bone Density
- Consume calcium-rich foods (dairy, leafy greens, sesame seeds).
- Ensure sufficient vitamin D exposure through sunlight or supplements.
- Get DEXA scans post-menopause for early detection of osteoporosis.
4. Be Pregnancy-Smart
- Use correct lifting techniques—bend at the knees, not the waist.
- Sleep with support pillows to reduce spinal pressure.
- Consult with a physiotherapist for pelvic and lumbar strengthening.
5. Manage Hormonal Health
- Consult gynecologists about HRT (Hormone Replacement Therapy) when appropriate.
- Avoid over-reliance on painkillers for menstrual back pain—explore long-term solutions like physical therapy or posture correction.
When to Seek Help: Signs You Shouldn’t Ignore
Back pain in women is often brushed off as fatigue, aging, or “normal.” But some signs indicate that it’s time to consult a spine specialist:
- Persistent or worsening back pain for more than a few weeks
- Pain radiating to the legs or arms (could indicate nerve involvement)
- Visible spinal curvature or posture issues
- Weakness, numbness, or tingling
- Difficulty standing or walking
- Pain related to pregnancy or childbirth that doesn’t resolve
At WeAreSpine, we use state-of-the-art diagnostic tools, including MRI, DEXA scans, and nerve conduction studies, to get to the root cause of back problems and treat them holistically.
The Importance of Early Diagnosis
Women are often caregivers—putting the health of others before their own. Unfortunately, this can lead to delayed diagnosis and prolonged suffering.
Benefits of Early Intervention:
- Prevent irreversible spine damage
- Avoid major surgery with early rehab or minimally invasive options
- Improve overall quality of life and functionality
- Enable active and independent aging
WeAreSpine’s outreach efforts, such as educational seminars, health camps, and personalized consultations, are aimed at catching these issues early.
Real Stories, Real Impact
Through our specialized women’s spine care programs, WeAreSpine has helped countless women regain control over their lives. From treating pregnancy-induced back problems to managing osteoporotic fractures and scoliosis, our focus has always been on minimally invasive treatment, long-term prevention, and ethical care.
Conclusion
Women face a unique set of risks when it comes to spinal health, thanks to biological, hormonal, and lifestyle changes. But back pain and spinal conditions don’t have to be accepted as a “normal” part of life. With early detection, personalized treatment, and preventive strategies, women can maintain a strong and healthy spine throughout life.
At WeAreSpine, we’re here to support women at every stage—from adolescence to menopause and beyond—with compassionate, evidence-based care.
If you or a loved one is struggling with back pain, don’t wait. Reach out to WeAreSpine today for a consultation and take the first step toward pain-free living.